Diabetes Gastroparesis: Symptoms, Causes, Diagnosis, and Treatment

Have you ever felt like your food was just sitting in your stomach for hours or felt bloated after eating only a small meal? For many people with diabetes, this can be a common experience. It could be a sign of diabetic gastroparesis, a condition where your stomach takes longer to digest food.
In this blog, we’ll talk about what diabetic gastroparesis is, why it happens, and some simple ways to manage it. Let’s start with knowing what diabetic gastroparesis is?
What is Diabetic Gastroparesis?
Diabetic gastroparesis happens when the stomach muscles don’t work properly because high blood sugar has damaged the nerves that control them.
Normally, your stomach muscles push food into your small intestine to continue digestion, but with gastroparesis, this process slows down or stops, making food stay in your stomach longer than it should.
What are the Symptoms of Diabetic Gastroparesis?
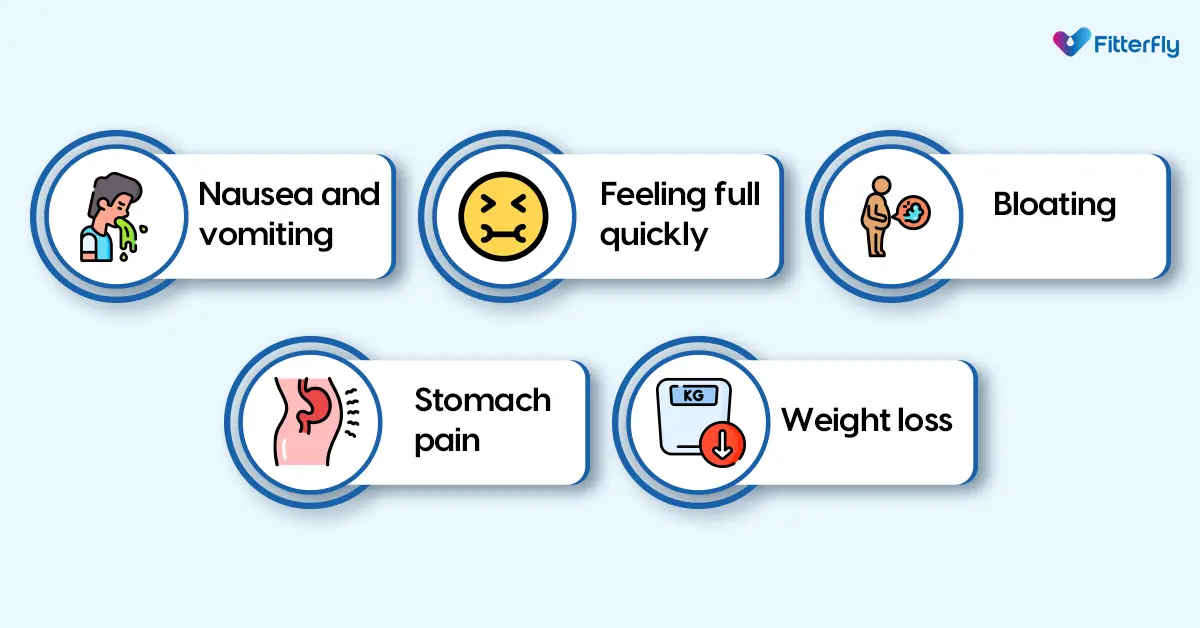
The symptoms of diabetic gastroparesis can vary, but some common signs to look out for include:
- Nausea and vomiting: You might feel queasy or even throw up after eating.
- Feeling full quickly: You may feel overly full even after eating a small amount.
- Bloating: Your stomach might feel swollen or puffed up.
- Stomach pain: You may experience discomfort or pain in your upper abdomen.
- Weight loss: Because your body isn’t getting enough nutrients from food, you might start losing weight unintentionally.
If you’re experiencing any of these symptoms regularly, speaking with your doctor is essential, as stomach problems caused by diabetes can often go unnoticed and untreated.
To know your chances of Diabetes reversal, take the Diabetes Reversal TestDiabetes Reversal
Calculator
What are the Causes of Diabetic Gastroparesis?
Diabetic gastroparesis is primarily caused by damage to the vagus nerve*, which controls the stomach muscles. High blood sugar levels over time can damage this nerve, leading to the development of gastroparesis.
Other factors that might contribute include:
- Having diabetes for many years: The longer you’ve had diabetes, the more likely it is to cause nerve damage. For example, if you’ve had diabetes for over 10 years, you may start noticing digestive issues.
- High blood sugar levels: Consistently high blood sugar over time can damage the nerves that help your stomach work properly. For instance, if your sugar levels stay high after meals, it can delay digestion.
- Smoking and alcohol: Both smoking and drinking can worsen nerve damage. For example, regular smokers may experience slower digestion because the nerves controlling their stomach muscles get affected.
- Stress and anxiety: Emotional stress can affect how your stomach functions, making symptoms more severe.
- Eating fatty or high-fiber foods: Foods like samosas, cheesy pizza, or burgers can take longer to digest, which can be a problem when your stomach is already slow in emptying.
- Certain medications: Some medicines, including those for diabetes, can slow down digestion. For example, drugs like certain insulin types or diabetes medications may have side effects that affect how quickly your stomach empties.
- Past surgeries: If you’ve had surgery around your stomach, such as gallbladder surgery or weight loss surgery, it could affect the nerves controlling digestion, making it slower.
- Thyroid problems: If your thyroid gland isn’t working properly (hypothyroidism), it can slow down your whole system, including your digestion. For example, people with thyroid issues often feel bloated and may have trouble digesting food quickly.
- Autoimmune conditions: Certain diseases, like lupus, can affect how your stomach muscles work. This means your stomach takes longer to move food through, which can worsen gastroparesis.
- Not drinking enough water: Dehydration can make your stomach slow. If you’re not drinking enough water during the day, especially in hot weather, it can slow down your digestion.
These are common causes of diabetes and stomach problems that people with diabetes often face, so it’s important to stay mindful of your diet, medications, and lifestyle choices.
*The vagus nerve is the longest cranial nerve, extending from the brainstem to the abdomen, part of the nervous system (autonomic nervous system).
| Did You Know?
The vagus nerve controls essential bodily functions like heart rate, digestion, and breathing, connecting the brain to major organs. |
What are the Complications of Diabetic Gastroparesis?
Diabetic gastroparesis can lead to other problems, such as:
- Malnutrition: Since your stomach doesn’t empty food properly, your body might not get enough nutrients.
- Unstable blood sugar levels: Gastroparesis can make it hard to control your blood sugar, causing sudden highs and lows.
- Bezoars: These are solid lumps of undigested food that can build up in your stomach and cause blockages.
How is the Diagnosis of Diabetic Gastroparesis Done?
It’s important to consult a gastroenterologist or with your doctor for an accurate diagnosis. Self-diagnosis should be avoided. Diagnosing diabetic gastroparesis involves a few steps, including:
- Medical history: Your doctor will review your symptoms and diabetes management history.
- Physical examination: They might check your abdomen for any signs of bloating or discomfort.
- Tests: You may undergo tests like a gastric emptying study (a test that measures how long it takes for food to leave your stomach) or an upper gastrointestinal endoscopy (a procedure to look at your stomach lining).
What are the Treatments for Diabetic Gastroparesis?
Treatment for diabetic gastroparesis focuses on managing symptoms and improving stomach function. Here’s how:
- Medications: Doctors may prescribe drugs to help stimulate stomach muscles or reduce nausea and vomiting.
- Blood sugar management: Keeping your blood sugar levels stable is crucial in managing gastroparesis.
- Diet changes: Changes in your eating habits can greatly help in managing symptoms (discussed below).
- Surgical options: In severe cases, surgery may be needed to help the stomach empty more effectively.
What are the Preventive Measures for Diabetic Gastroparesis?
Preventing diabetic gastroparesis is all about managing diabetes effectively. Here are some steps you can take:
- Monitor blood sugar regularly: Keeping your levels within the target range helps prevent nerve damage. Regular follow-ups with your doctor are key to adjusting your treatment as needed.
- Follow your diabetes care plan: Stick to your prescribed medications, diet, and exercise routines. If necessary, your doctor may change your therapy or medication, so attending regular check-ups is essential.
- Stay informed: Educate yourself about diabetes and its complications. Recognise early signs of problems and consult your healthcare provider right away if you notice any new or worsening symptoms
What are the Dietary and Lifestyle Changes for Managing Diabetic Gastroparesis?
Managing diabetic gastroparesis involves not just careful diet changes but also regular exercise and consistent monitoring of your condition. Here are some tips to help alleviate symptoms:
1. Opt for smaller, more frequent meals
Eating smaller portions more often can reduce the workload on your stomach. Instead of three large meals, try having smaller, diabetes-friendly portions like a bowl of moong dal cheela, a small portion of upma made with millets, or plain dahi/yoghurt with a handful of nuts at different times throughout the day.
2. Choose easily digestible foods
Low-fat and low-fiber foods are easier for your stomach to process, reducing discomfort. Opt for soft, well-cooked vegetables like lauki (bottle gourd) or tinda (Indian round gourd), and light dals like moong dal, which are gentle on the stomach and good for blood sugar control.
3. Avoid high-fat and high-fiber foods
These can slow down digestion even further and worsen symptoms. It’s best to limit fried snacks, high-fiber rotis (like those made with bajra or jowar), and oily gravies. Instead, choose plain chapati or steamed vegetables.
4. Stay hydrated
Drink plenty of fluids like water, chaas (buttermilk without added sugar), or nimbu pani (lemon water without sugar). Avoid carbonated drinks, as they can cause bloating.
5. Chew food thoroughly
Chewing your food well helps your stomach process it more easily. For example, take time to chew chapati with sabzi thoroughly before swallowing.
6. Consider liquid meals
If solid foods are too uncomfortable, try lighter options like soups, thin dals, or smoothies made with diabetes-friendly fruits like guava or apples.
7. Exercise for Gastroparesis Management
Light physical activity, like a 10-15 minute walk after meals, can help stimulate digestion and keep food moving. Regular exercise, such as yoga or light aerobics, can further improve digestion and blood sugar control.
Always consult your doctor before starting any new exercise routine, especially if you have diabetes-related complications.
How We At Fitterfly Can Help You?
At Fitterfly, we recognize that managing diabetic gastroparesis alongside diabetes can feel overwhelming, but it doesn’t have to be. Our personalized approach ensures that you receive the right support at every step.
We start by helping you create a meal plan that suits your unique needs, focusing on smaller, easy-to-digest meals that help ease the discomfort associated with gastroparesis. Alongside tailored nutrition, our health experts work closely with you to keep your blood sugar levels stable, which is crucial for managing gastroparesis effectively.
Beyond diet, we emphasize lifestyle changes like incorporating light exercises that promote digestion and overall well-being. You’ll also have access to our advanced tracking tools in our fitterfly app, so you can monitor your progress in real-time and make informed decisions about your health.
Just give us a missed call at 08068507599, and we will get back to you!
Reduced HbA1c by HALF in 6 months


6.6%
Happy members
EMI
Guarantee
4.8/5
Diabetes Prime Program
This blog provides general information for educational and informational purposes only and shouldn't be seen as professional advice.