The Complete Guide to Hypoglycemia (Low Blood Sugar)
Living with diabetes brings its own set of hurdles, and one such challenge is the presence of hypoglycemia, commonly known as low sugar.
Whether you have Type 1 or Type 2 diabetes, managing your blood sugar levels becomes a delicate balancing act. The fear and anxiety accompanying hypoglycemia episodes can hinder your ability to achieve optimal control and reach your health goals.
However, with the right knowledge, plan, and support, you can take charge and prevent these low-sugar episodes from disrupting your daily life.
In this article, you will learn about diabetes and hypoglycemia in detail, how to avoid them, and what you can do if you experience it.
What exactly is Hypoglycemia or Low sugar?
Hypoglycaemia, also known as low sugar, is a common symptom experienced by people with diabetes, regardless of whether they have Type 1 or Type 2 diabetes mellitus. It occurs when the glucose concentration in the blood drops below 70mg/dl, which can potentially harm the patients.
Severe low blood sugar is when it goes below 54 mg/dl; at this point, the individual may require assistance to treat the episode.
It can also occur when taking oral medications or insulin injections as part of their treatment.
Apart from that, the episodes of hypoglycemia bring physical and psychological challenges like fear and anxiety. This fear becomes a barrier, making it hard for patients to control their blood sugar levels and reach their goals.
Lack of awareness, called hypoglycemia unawareness, can be dangerous and reduce the quality of life. So, educating patients is key to prevention.
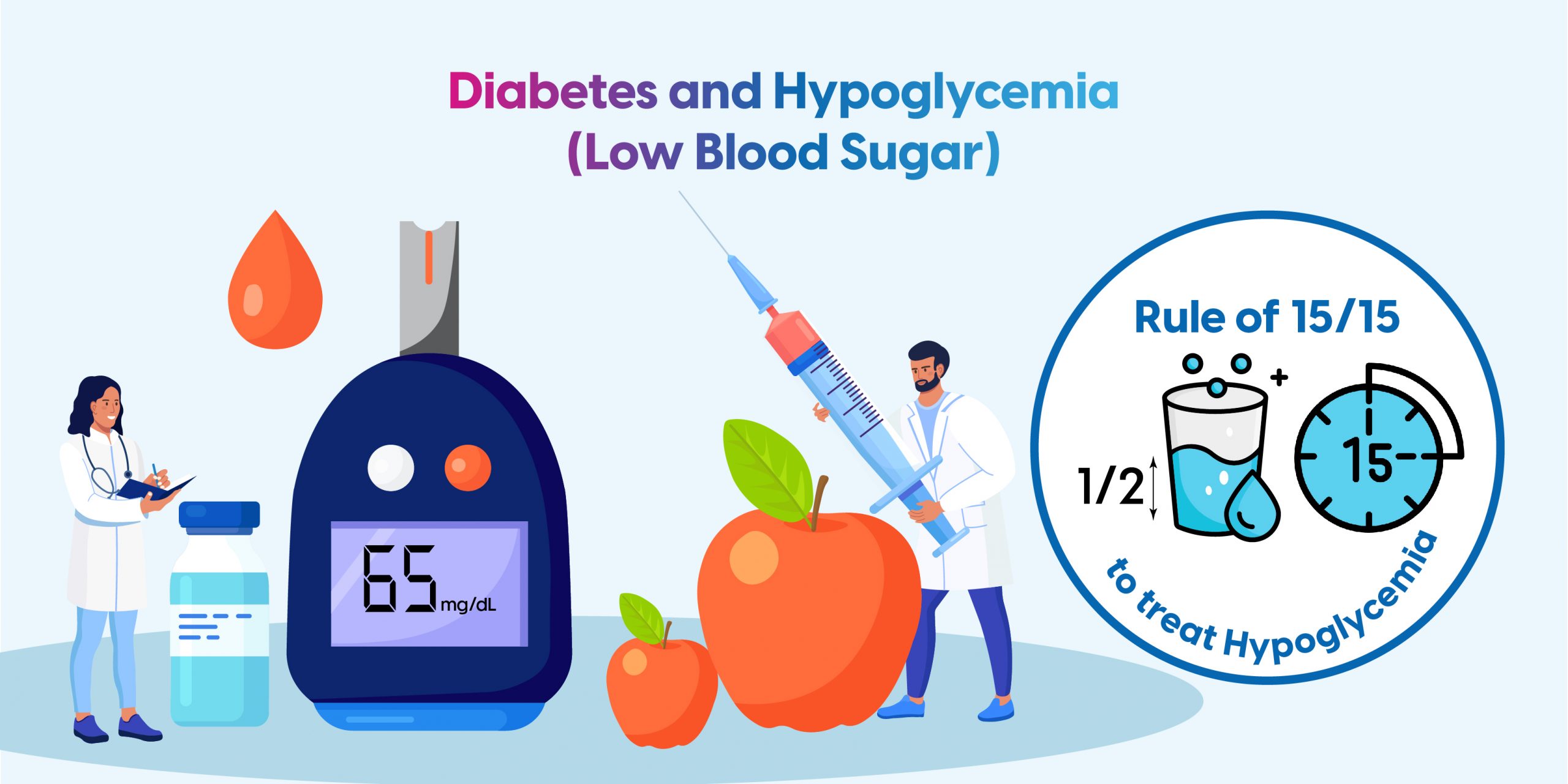
What are the Signs and Symptoms of Hypoglycemia?
The signs and symptoms of hypoglycemia can vary among patients, depending on their age, duration of diabetes and severity of hypoglycemia.
For example, children may experience emotional and behavioural changes alongside classic autonomic and neuroglycopenic symptoms.
- Autonomic symptoms related to the involvement of the autonomic nervous system include anxiety, trembling, palpitations, sweating, and feeling hungry.
- Neuroglycopenic symptoms, caused by the brain’s glucose deprivation, include lack of concentration, headaches, blurred vision, dizziness, confusion, convulsions, speech difficulties, restlessness, and even loss of consciousness.
**Such hypoglycemia signs and symptoms are usually observed when blood sugar levels drop around 54 mg/dL.
What are the Causes of Hypoglycemia?
Hypoglycemia occurs when your blood sugar levels drop below normal (less than 70 mg/dL). This can be due to various factors, including:
- Reactive Hypoglycemia: Occurs after meals when the body produces too much insulin.
- Fasting Hypoglycemia: This happens when you haven’t eaten for a long time.
- Drug-Induced Hypoglycemia: Caused by medications, especially insulin or oral diabetes drugs.
- Medical Condition-Related Hypoglycemia: Some of the illness in your body, like liver disease, kidney disorders, or hormonal deficiencies, can also cause hypoglycemia.
- Excessive alcohol consumption
- Intensive physical activity without adequate food intake
What are the Types of Hypoglycemia?
There are several types of hypoglycemia, each with different causes:
- Reactive Hypoglycemia: Occurs after eating, usually within a few hours. It can be due to excessive insulin production.
- Fasting Hypoglycemia: This happens when you haven’t eaten for a while, often seen in people with certain medical conditions.
- Drug-Induced Hypoglycemia: Caused by medications, especially those used to treat diabetes.
- Medical Condition-Related Hypoglycemia: Certain illnesses, such as liver disease, kidney disorders, or hormonal deficiencies, can also cause hypoglycemia.
What are the Risk Factors for Hypoglycemia?
Several risk factors contribute to the occurrence of hypoglycemia. These include:
- Taking high doses of insulin or oral drugs like sulfonylureas or glinides, especially if not timed correctly with meals.
- Consuming very low-carbohydrate meals or fasting for long periods can limit the body’s ability to produce glucose.
- Experiencing hypoglycemia after engaging in heavy physical exercise.
- Experiencing a decrease in insulin excretion due to conditions like kidney failure, liver failure, or thyroid problems.
To know your chances of Diabetes reversal, take the Diabetes Reversal TestDiabetes Reversal
Calculator
What are the Complications of Untreated Hypoglycemia?
Untreated hypoglycemia can affect your quality of life, such as:
- Loss of memory
- Persistent fatigue, tiredness
- Unable to work
- Increased risk of accidents and injuries
If untreated, it can lead to serious complications. Some of them are:
- Loss of consciousness
- Seizures
- Brain damage
When to Seek Medical Help for Hypoglycemia?
Whenever you find you are having hypoglycemia, seek immediate medical attention if you experience:
- Persistent low blood sugar despite eating or drinking something sugary
- Severe confusion or loss of consciousness
- Seizures
- Recurrent hypoglycemia
- Hypoglycemia without symptoms (needs medication dose adjustment)
How to Diagnose Hypoglycemia?
Diagnosing hypoglycemia typically involves:
- Reviewing symptoms and medical history
- Glucometer – spot diagnosis in an emergency situation
- Lab Blood tests to measure blood sugar levels, HbA1c
- Monitoring blood sugar over time using continuous glucose monitoring (CGM) systems
What are the Effects of Hypoglycemia?
Hypoglycemia can cause both physical and psychological issues for diabetic patients. It can impair judgment, affect daily activities such as driving, learning, concentration and impact behaviour.
It may lead to convulsions, loss of consciousness, and even transient neurological deficits or stroke in severe cases. Repeated episodes of hypoglycemia can result in a lack of warning symptoms, referred to as Hypoglycemia unawareness.
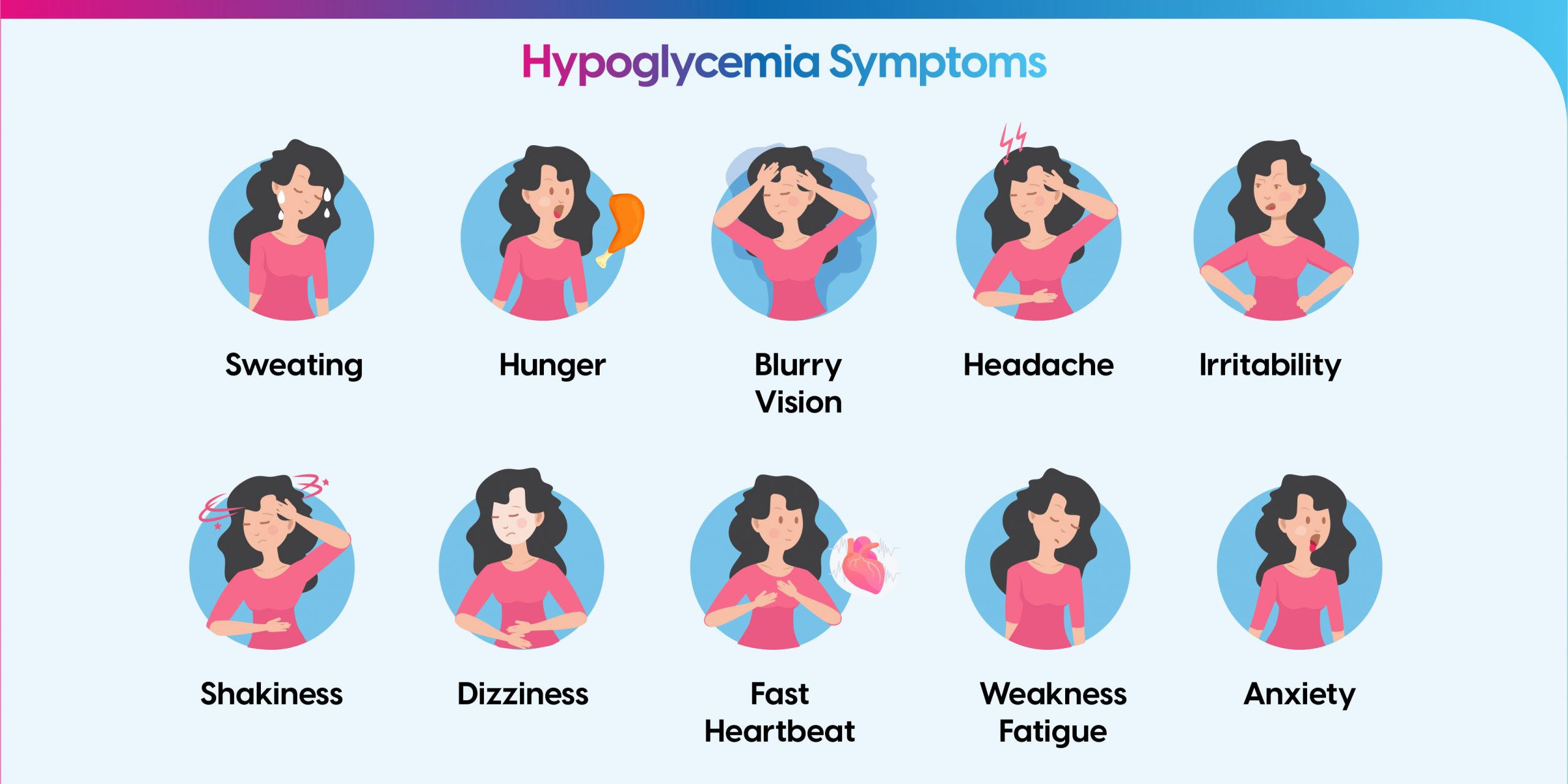
What is the Treatment of Hypoglycemia?
There is a practical approach known as the “Rule of 15” that can help manage low blood sugar (Hypoglycaemia) effectively. Here’s how it works:
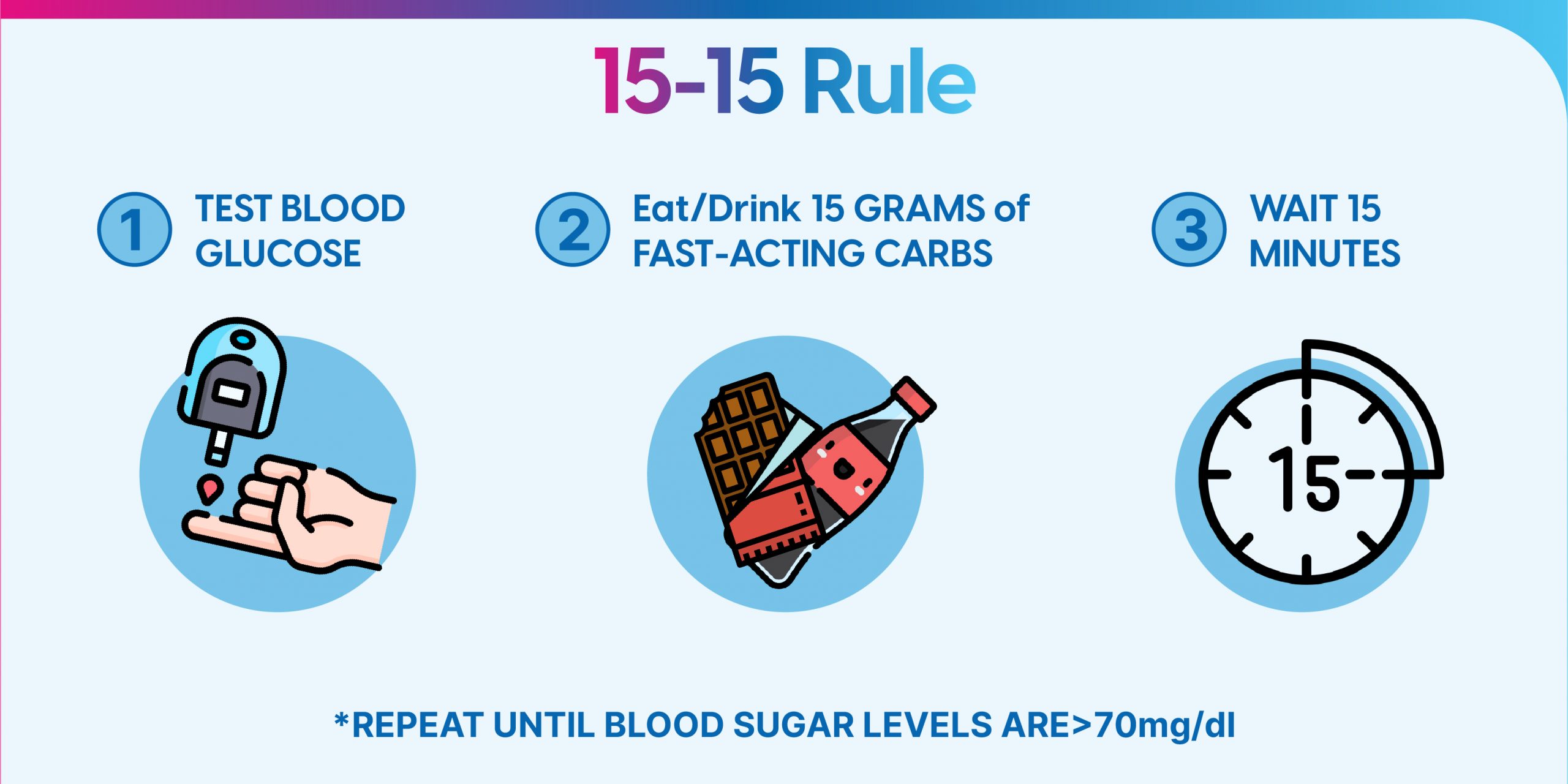
The Rule of 15:
1. Check your blood sugar levels using a glucometer to ensure they are below 70 mg/dL, indicating hypoglycemia.
2. Now, consume 15 grams of carbohydrates to increase blood sugar levels. E.g., 15 grams of glucose powder, 3 glucose biscuits, 3 hard candies, 150 ml of fruit juice (without added sugars) etc.
3. Wait for 15 minutes to allow the carbohydrates to be absorbed and raise your blood sugar levels.
4. After 15 minutes, recheck your blood sugar levels to assess if they have risen above 90 mg/dL (this is the target range to aim for).
**Repeat if necessary: If your blood sugar is still below 90 mg/dL, repeat the initial step, and wait for another 15 minutes
5. Once your blood sugar rises above 90 mg/dL, consuming a balanced meal or snack is essential to provide sustained energy and prevent a subsequent drop in blood sugar levels.
Remember, the Rule of 15 is a guideline for managing low blood sugar levels, and it’s essential to consult with healthcare professionals for personalised advice on managing diabetes and hypoglycemia.
How to Prevent Hypoglycaemia?
1) Patient Education: Know the Signs and Take Action
- Make sure you and those around you can spot the symptoms of hypoglycemia.
- Discuss the risks and treatment options with your healthcare provider.
- Identify potential triggers, like missed meals, intense exercise, or alcohol consumption.
- Carry glucose or carb-rich snacks to tackle low blood sugar on the go.
2) Smart Eating: Balance Carbohydrates for Blood Sugar Control
- Understand the impact of carbohydrates on blood glucose levels.
- Create a personalised meal plan with a focus on insulin timing and dosage.
- Always keep glucose or carb-containing foods readily available.
- Consider a bedtime snack to prevent nighttime hypoglycemia, especially for type 1 diabetes.
3) Exercise with Caution: Manage Blood Sugar during Physical Activity
- Monitor your blood sugar levels before and after workouts.
- Take precautions to prevent hypoglycemia, such as eating small meals beforehand.
- Carry fast-acting carbs or glucose during exercise sessions.
- Adjust insulin doses based on your planned physical activity.
4) Stay on Top with Glucose Monitoring: Catch Hypoglycemia Early
- Regularly check your blood glucose levels using self-monitoring.
- Test before meals, after meals occasionally, before sleep or at 3 am, before demanding tasks like driving, after treating hypoglycemia, and when suspecting low blood sugar.
- Consider continuous glucose monitoring (CGM) for real-time glucose measurement.
5) Medication Adjustment: Minimize Hypoglycemia Risk
- Once diagnosed with diabetes, talk to your doctor and maintain proper follow-ups.
- Avoid self-medications or dose modification.
- Use home remedies with caution.
- Discuss alternate options for insulin and its analogues to reduce hypoglycemia.
- Evaluate the need to reduce or discontinue medications.
By following these practical strategies, you can actively prevent hypoglycemia and maintain stable blood sugar levels. Remember, staying informed and taking proactive steps are key to achieving your diabetes management goals.
FitterTake
Understanding hypoglycemia is vital for effective diabetes management. It’s as important as achieving blood sugar control and hitting target levels. However, at some point, nearly every person with diabetes encounters hypoglycemia.
But that can be manageable if you follow prevention strategies such as smart eating habits, careful exercise management, regular glucose monitoring, and medication adjustment. You can actively prevent hypoglycemia and maintain stable blood sugar levels.
With Fitterfly’s Diabetes Care Program, we offer a diabetes management program designed by a comprehensive team consisting of a nutrition coach, a physiotherapy coach, and a success coach.
By doing so, we can minimize the risks and consequences of hypoglycemia, leading to better overall diabetes management. Speak to us and book a free consultation to learn more about how we can support you or just give us a missed call at 08068507599
Reduced diabetes medications in 3 months


6.8%
Happy members
EMI
Guarantee
4.8/5
Diabetes Prime Program
This blog provides general information for educational and informational purposes only and shouldn't be seen as professional advice.
Frequently Asked Questions
Why is hypoglycemia dangerous?
Hypoglycemia can be dangerous as it can lead to serious complications, especially if blood glucose stays low for too long, including seizures, loss of memory, loss of consciousness and can be life-threatening in some rare cases.
How does hypoglycemia occur?
Hypoglycemia occurs when the glucose levels in your blood drop below the normal range, typically less 70 milligrams per deciliter (mg/dL) and if it is less than 54 mg/dL it is termed as severe hypoglycemia.
How is hypoglycemia diagnosed?
Hypoglycemia can have some symptoms which can be confirmed with blood test. To diagnose hypoglycemia accurately, healthcare providers may perform the lab tests such as: Blood Glucose Testing - with a glucometer or a lab. In case of hypoglycemia in people without diabetes needs a detailed clinical evaluation.
What triggers hypoglycemia?
It can be triggered when you not eating enough, postponing or skipping a meal or snack, increasing exercise or physical activity or without eating or self-adjusting medications, and drinking alcohol.
Can hypoglycemia cause death?
In severe cases, hypoglycemia can indeed be life-threatening if untreated for long.
How low is hypoglycemia?
Hypoglycemia is typically when your blood sugar reading lower than 70 milligrams per deciliter (mg/dL) and severe if the reading is less than 54 mg/dL.
What is the Difference Between Hypoglycemia and Hyperglycemia?
Hypoglycemia refers to low blood sugar levels, while hyperglycemia means high blood sugar levels. Both conditions can be lead to several health issues if not managed properly.
Can You Have Hypoglycemia Without Diabetes?
Yes, it's possible to experience hypoglycemia without having diabetes. Causes can include certain medications, excessive alcohol consumption, and underlying health conditions like kidney problems and hormonal disbalance.
What to Eat When Blood Sugar is Low?
If your blood sugar is low, quickly consume 15-20 grams of fast-acting carbohydrates, such as glucose tablets, fruit juice, or regular soda. Follow up with a snack containing protein and complex carbohydrates to stabilize your blood sugar.
Is it Safe to Sleep with Low Blood Sugar?
Sleeping with low blood sugar is not safe as it can lead to severe hypoglycemia. If you suspect low blood sugar before bed, treat it with fast-acting carbohydrates and monitor your levels.
Can Hypoglycemia Cause a Heart Attack?
Severe hypoglycemia can affect your heart health and can cause heart-related issues. It's important to manage blood sugar levels to reduce such risks.
Will Hypoglycemia Cause Weight Gain?
Frequent low blood sugar episodes might increase calorie consumption, contributing to weight gain.
Why Does Hypoglycemia Occur in Diabetes?
Hypoglycemia in diabetes can result from taking too much insulin, not eating enough carbohydrates, or exercising more than usual without adjusting food intake or medication.
Why Does Hypoglycemia Cause Seizures?
Severe hypoglycemia deprives the brain of glucose, its primary energy source, leading to neurological symptoms like seizures. Prompt treatment is essential to prevent such severe complications.
How Common is Hypoglycemia?
Hypoglycemia is relatively common, particularly among people with diabetes who use insulin or other oral medications and sometimes skip their meals or do strength exercises or fail to monitor and consult with their doctor regularly, add dose adjustments, develop other complications due to diabetes, etc. It can also affect people without diabetes, though this is less frequent.
Who is at a Higher Risk of Developing Low Blood Glucose?
People at a higher risk of developing low blood glucose include those with diabetes who are on insulin or certain oral medications, especially if they fail to monitor their blood sugar levels properly. People with a history of hypoglycemia unawareness are also at increased risk, as are those with certain medical conditions that affect hormone levels or organ function.