What is Diabetic Neuropathy? Types, Causes, Symptoms and How to Prevent It

Have you ever felt a sudden tingling, pain, or numbness in your hands, arms, and feet?
Most of us think that such conditions could be due to other conditions, but do you know this could be a warning sign of diabetic neuropathy if you have type 2 diabetes that’s not well-managed.
It’s important not to overlook these symptoms.
This problem can start in your arms and legs, but it can also affect important organs such as stomach, bladder, and heart if you don’t take care of it. And it’s not just about sugar – too much fat in your body can make it worse too.
So exactly, What is Diabetic Neuropathy? Keep on reading we have simplified all your queries.
What Is Diabetic Neuropathy?
Diabetic neuropathy is a condition where there is damage to the nerves caused by high blood sugars in people with Diabetes.
What Causes Diabetic Neuropathy?
- Damage to nerves due to Long duration of uncontrolled diabetes
- High sugars can even damage small blood vessels in people with diabetes and cause nerve damage later
- Not only high sugars, even high cholesterol, but high BP in the blood can also damage nerves
Types of Diabetic Neuropathy and Symptoms
There are mainly four types of diabetic neuropathy:
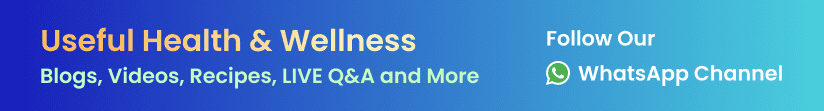
1. Peripheral Neuropathy
This type of neuropathy is very common, affecting your hands and feet. About one-third to one-half of people with diabetes have peripheral neuropathy.
Symptoms
- Tingling and numbnes sensation or pain
- Burning sensation
- Unable to feet heat or cold sensation
- Unable to feel any injury
- Problems with balance
- Muscle loss in limbs (hands & legs)
- Can affects joints in the feet, also known as Charcot’s joint
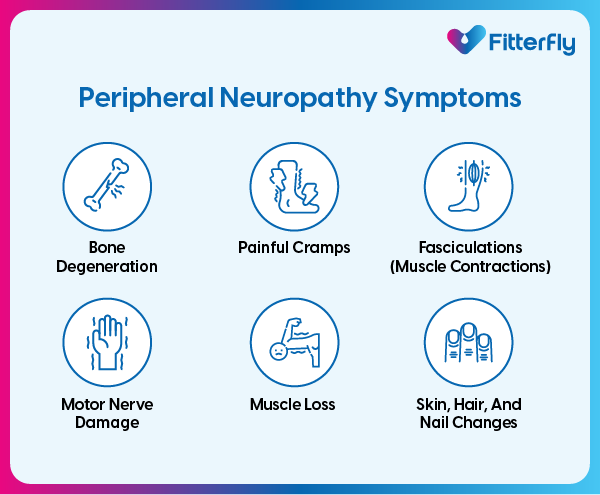
2. Autonomic Neuropathy
Autonomic neuropathy is damage to nerves that control your internal organs, leading to problems in specific organs such as
- Heart affecting your heart rate and blood pressure,
- Digestive system,
- Urinary bladder,
- Sex organs,
- Sweat glands, and eyes.
- The damage can also lead to hypoglycemia unawareness.
Symptoms
- Faster heart rate
- Feeling dizzy, or giddiness
- Urinary complaints like-Dribbling or retention of urine in bladder
- Bloating, acidity, vomiting, diarrhea or constipation
- Sexual dysfunction
- Excessive sweating
- Frequent hypoglycemia without symptoms
3. Focal Neuropathy
This is due to damage to a single nerve.
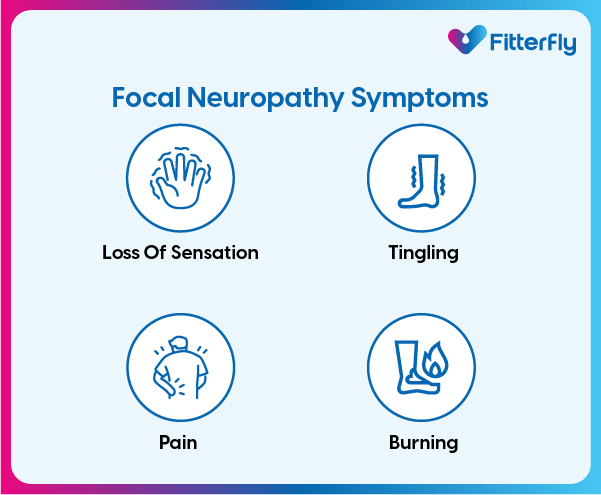
Symptoms
As per the nerve involved, can lead to
- Loss of sensation
- Tingling
- Pain
- Burning in affected nerve
4. Proximal Neuropathy
Proximal neuropathy is a rare and disabling type of nerve damage in your hip, buttock, or thigh.
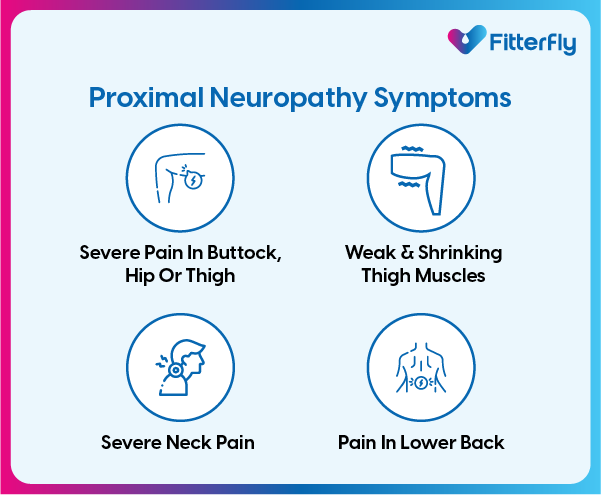
Symptoms
- Can affect the neck
- Lower back
- Shoulder area
- Nerve damage in your hip, buttock, or thigh, etc.
How is Diabetes-related Neuropathy Diagnosed?
Diabetes-related neuropathy is diagnosed through a combination of clinical and specific tests to determine the extent and type of nerve damage.
It can be done:
Clinically at the hospital
- Tests including: Physical examination of your feet, touch, temperature, joint position, and vibration.
- Foot pressure test, Microfilament test, biosthesiometry etc.
- If your doctor suspects nerve damage, then an electromyogram (EMG) or Nerve Conduction Velocity (NCV) test will be done to measures your nerve response.
- If autonomic diabetic neuropathy (ANDR) is suspected, additional tests are performed like: Heart Rate Variability Tests, Gastrointestinal Tests, Bladder Function Tests, Sweat Tests, etc.
What are the Complications due to Diabetic Neuropathy?
Diabetic neuropathy commonly affects feet and can cause
- Sores and ulcers or infections in the feet
- Loss of balance and coordination, leading to falls and fractures
- Amputations
- Long-standing pain
- Psychologically can lead to anxiety and depression
Autonomic neuropathy, can affect organ function, and cause issues with heart rate, blood pressure, digestion, urination, and sensing low blood glucose.
To know your chances of Diabetes reversal, take the Diabetes Reversal TestDiabetes Reversal
Calculator
How is Diabetes-related Neuropathy Treated?
Early diagnosis and management
Early diagnosis and management is the key to prevent complications
It is important to keep blood sugars under control through-:
- Eating a nutritious diet.
- Exercising regularly.
- Taking all diabetes medications as prescribed.
Once diagnosed your health care provider may manage diabetes-related neuropathy symptoms with
- Pain medicines, including topical creams or patches.
- Other medications can reduce pain.
You should also check your feet daily for wounds or injuries.
How can I Prevent Diabetic Neuropathy from getting worse?
To prevent the worsening of diabetic neuropathy, adopt a holistic approach that includes strict diabetes control and lifestyle changes.
- Keep blood sugar, pressure, and cholesterol in check.
- Exercise regularly (like walking or swimming) to control blood sugar and boost health.
- Eat balanced diet, avoid fad diet.
- Reduce alcohol and stop smoking to enhance circulation and reduce neuropathy risk.
- Take all diabetes medications as prescribed.
- Check your feet daily and get regular foot and nerve check-ups.
How We At Fitterfly Can Help You?
Prevention over cure is the best approach to diabetes-related complications like diabetic neuropathy. Regularly testing your blood sugar levels is important to prevent this condition from developing or progressing.
If you have a family history of diabetes or have been diagnosed with prediabetes, you must proactively get your blood sugar levels tested once every few months (based on your doctor’s recommendations.
Once you know a diagnosis, consult your doctor and find a scientific and comprehensive diabetes reversal or management plan.
Fitterfly’s various Diabetes Prime Program have been designed by India’s top diabetologists, nutritionists, fitness experts and psychologists and have helped over 25000+ Indians effectively manage their diabetes.
If you need help with more information on diabetic neuropathy or wish to control your blood sugar levels, speak to us by just giving a missed call at 08068507599.
Reduced HbA1c by HALF in 6 months


6.6%
Happy members
EMI
Guarantee
4.8/5
Diabetes Prime Program
This blog provides general information for educational and informational purposes only and shouldn't be seen as professional advice.
Frequently Asked Questions
What Is the Best Treatment for Diabetic Neuropathy in Feet?
The best treatment often includes a combination of approaches. Keeping blood sugar levels well-controlled is crucial. Regular exercise and foot care are also key. Get in touch with your diabetologist or a neurologist to understand your condition and how you can manage it well.
What Is Diabetic Neuropathy in the Feet?
Long standing-uncontrolled diabetes can affect either a single or multiple nerve commonly in he feet which can lead to symptoms of diabetic neuropathy in the feet. It can lead to pain, tingling, weakness, or numbness in the feet and legs.
What A1C Level Causes Neuropathy?
There's no specific A1C level that "causes" neuropathy, but higher levels over time increase the risk. Keeping A1C levels below 7% over a period of time it can help to reduce the risk of developing neuropathy.
Can diabetes-related neuropathy be reversed?
Maybe. You can keep diabetes-related neuropathy from worsening, and you may be able to reverse nerve damage with very good management of blood glucose, but the process is very slow.
What Are the Common Signs of Diabetic Neuropathy?
The signs of diabetic neuropathy include numbness, tingling, or pain in the extremities, particularly the feet and hands. Some people may experience extreme sensitivity to touch, muscle weakness, or loss of balance and coordination.
How Is Diabetic Neuropathy Diagnosed?
Diagnosis of diabetic neuropathy typically involves a comprehensive physical exam, discussions of symptoms, and specific tests that may include nerve conduction studies and electromyography. These assessments help your doctor to understand the extent of nerve damage and formulate an appropriate treatment plan.
What is the Treatment for Diabetic Neuropathy?
While a cure for diabetic neuropathy remains difficult, but it can be managed. Usually, the treatment strategies often focus on controlling blood sugar levels to slow the progression of nerve damage, using medications to relieve pain, and adopting lifestyle changes to support overall health.
When to See Your Doctor?
If you notice signs of diabetic neuropathy or any changes in symptoms, immediately consult with your healthcare provider. Early intervention can prevent the condition from worsening and help maintain quality of life.