How DTx Provides the Missing Piece in Diabetes Management- CONSISTENCY!

“Doctor, we just can’t do it! It’s too tough. There are too many things to remember, the doses of the medicines are confusing and we don’t have the time to do exercise daily.”
Does this sound familiar? Have you had patients diagnosed with diabetes, who are frustrated with the lack of progress they are making? This type of response is not surprising because studies have shown that 90% to 95% of diabetes care requires self-care. The problem with compliance arises when patients are unable to keep up with the level of self-care required for treatments to work.
In this article you will read about:
- Monitoring Diabetes: Is it a question of commitment?
- Extending a Helping Hand
- It’s all about taking small steps to achieve big goals!
- Digital Therapeutics as an Ally
Monitoring Diabetes: Is it a question of commitment?
The American Association of Diabetic Educators (AADE) has identified 7 key patient behaviours that when followed, ensure good results. These include:
- healthy eating
- being physically active
- monitoring of blood sugar
- compliant with medications
- good problem-solving skills
- healthy coping skills
- risk-reduction behaviours
When we put ourselves in the patient’s shoes, we have to ask – is it truly a lack of motivation on their part, or are they missing an essential piece of the puzzle?
Extending a Helping Hand
As healthcare providers, how can we go beyond our clinic walls to get patients the care and guidance they need? Steps that go beyond testing, diagnosing, prescriptions and advice?
In an effort to get patients to comply with treatment plans, here are a few techniques that have shown great results:
1. Teamwork makes the dream work!
Getting a multidisciplinary team of providers from all fields to treat the patient holistically – from physical and mental wellbeing to nutritional habits, lifestyle factors and exercises, have shown great results.
2. Getting Up Close and Personal!
Considering that there is no “one size fits all” model in diabetes, a tailor-made approach is just what patients need! Every patient has a different health literacy level and may not have access to foods required for a complete diet change. This is when a personalised approach works! It may be as simple as:
- giving ideas for alternative foods
- an easier way to get their body moving
- a simple resource for clearing their doubts
3. Showing them the ropes!
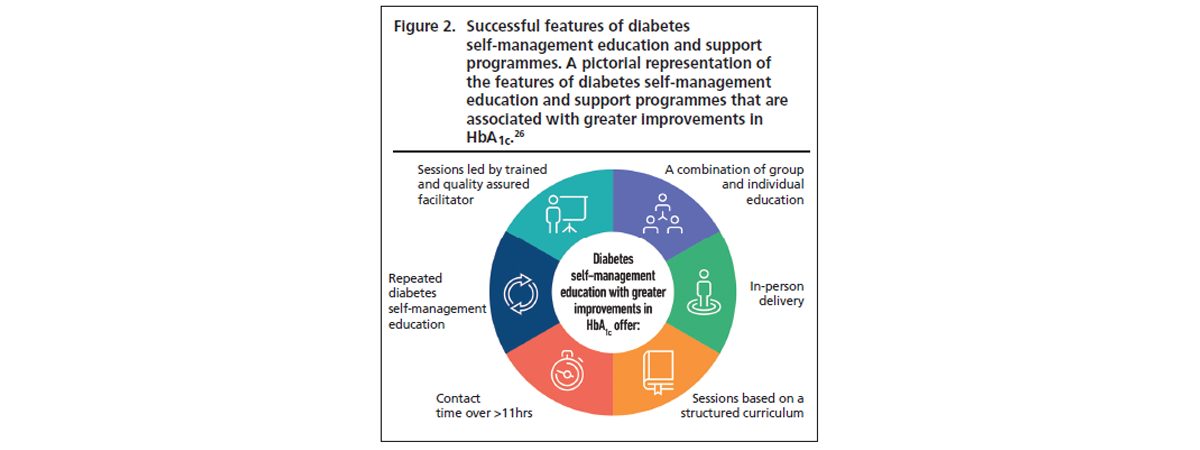
Educating patients about how to effectively manage their condition has been effective in getting them comfortable and more compliant with their treatments. A study in the British Journal of Diabetes illustrated the hallmarks of an effective diabetes self-management education (DSME) program, in the figure below.
Consistent Action Creates Consistent Results
However, even if targeted and team-based approaches are offered to patients, the key ingredient to great clinical outcomes still lies in CONSISTENCY!
It’s all about taking small steps to achieve big goals!
We know that continuous monitoring of blood sugar levels, activity levels and tracking calories can be overwhelming for patients. However, lifestyle therapy cannot be limited to just diet and exercise. Studies have shown that patients need the right mental and emotional support to stay motivated and resilient through the ups and downs of dealing with a chronic condition like diabetes.
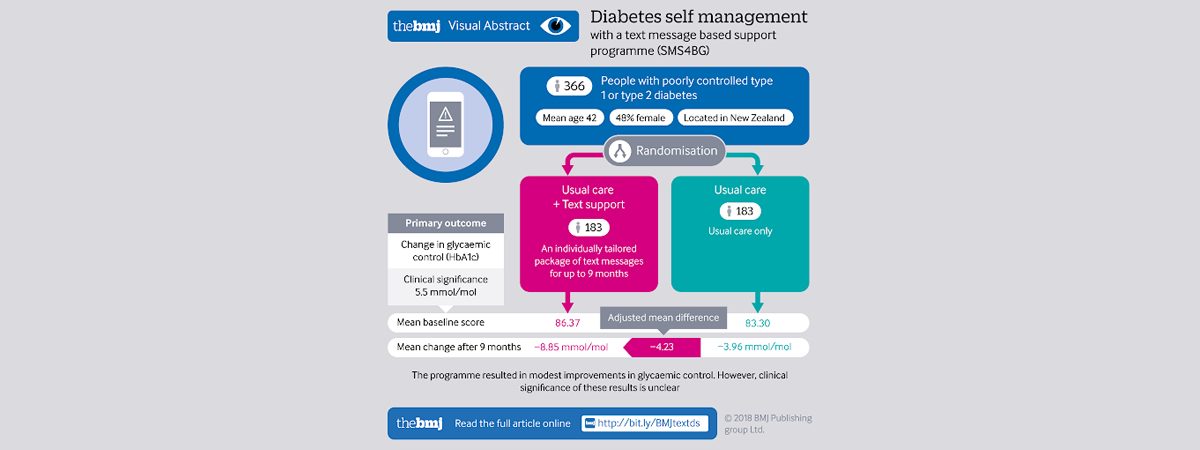
Recent research in the British Medical Journal highlighted the importance of consistent follow-up with patients for good clinical outcomes. They were divided into control and intervention groups where the intervention group received a tailored package of text messages for up to nine months in addition to the usual care provided to the control group. This offered information, support, motivation, and reminders related to diabetes self-management and lifestyle behaviours. At the end of the study period, patients in the intervention group enjoyed a significantly greater reduction in HbA1C levels than those in the control group.
Time for some Hard Truths
While consistent personal follow-up is a lofty goal in an ideal world, the ground reality is that very few physicians are able to keep up with the demands that come with long-term diseases like diabetes.
How long can clinicians handhold patients through their treatment journeys? Is there a way to keep them consistently engaged in their health, in an efficient way?
Digital Therapeutics as an Ally
Physicians are now recognizing the importance of leveraging digital therapeutics when helping their patients navigate their treatment plans.
Our previous blog explored the powerful partnerships that are formed when doctors team up with digital therapeutic models globally as well as in India.
At Fitterfly, we believe in filling the gap between clinic visits and consultations by helping people with diabetes make lifestyle changes that are essential for achieving blood glucose control and preventing complications.
Why does this approach work?
Because it is rooted in empathy, engagement and cutting edge health technology, a combination that brings outstanding outcomes!
How do we do it?
- We use personalized glycemic responses from AGM/ AGP or 20-point SMBG values to give recommendations for food, exercise and sleep.
- We guide our patients through their journey with diabetes – from macro and micronutrient deficiencies and hypoglycemia episodes to high glycemic variability.
- Our coaches interact personally with patients via calls and chats to nudge them towards making the right choices.
If you are interested in providing your patients with the best post clinic care to keep them consistent in their goals, click here to find out more about our personalised digital therapeutics programs!
This blog provides general information for educational and informational purposes only and shouldn't be seen as professional advice.
Don’t struggle alone & get the expert care you deserve













