Mastering Insulin Therapy in T2DM through Fitterfly’s Expert Discussion

Insulin therapy is one of the most crucial approaches to managing diabetes. Since the discovery of insulin in 1921 by Frederick Banting and Charles Best and 14-year-old Leonard Thompson emerging as the first individual to receive insulin injection, there has been a vast paradigm shift in the evolution of guidelines for uses of insulin.
To have a comprehensive grasp of insulin therapy, Fitterfly conducted an interactive discussion led by Dr. Tejal Lathia (MBBS, MD, DM-Endocrinology) in conversation with Dr. Neelesh Bhandari (Vice President-Physician Partnerships, Fitterfly).

Fig 1: Dr. Tejal Lathia, Leading Diabetologist, Navi Mumbai
The focal points of the discussion titled Mastering Insulin Therapy: Practical Insights for T2DM are encompassed below:
Type 2 Diabetes Clusters in India
Traditionally, scientists classified diabetes under two broad categories: Predominant Insulin Resistant diabetes and Predominant Insulin-deficiency diabetes. Individuals diagnosed with insulin-resistant diabetes are usually obese, manifest a sedentary lifestyle and experience stress and sleep disturbances.
On the contrary, individuals exhibiting insulin deficiency diabetes mostly have standard or lower body weight, show a strong family history of diabetes and test positive for autoimmune diabetes (GAD antibody).
Recently, researchers have identified different subtypes or “clusters” of Type 2 diabetes, each with its own set of symptoms and risks. In India, a study on over 19,000 individuals found four main clusters of type 2 diabetes, two of which were unique to Indians. Identifying these clusters enables a more accurate classification of diabetes types, guides physicians in selecting the most effective treatments and brings us a step closer to personalised diabetes care.
These clusters include:
1. Mild-Age Related Diabetes (MARD)
MARD constitutes 35.8% of the population living with diabetes in India. This cohort is characterised by advanced age, elevated HDL cholesterol, and C-peptide levels, with a reduced propensity for diabetic complications.
2. Severe Insulin Deficient Diabetes (SIDD)
SIDD is observed in 26.2% of cases. Patients in this category are typically diagnosed at a younger age and exhibit low Body Mass Index (BMI) and waist circumference, alongside elevated HbA1c levels. They are at an increased risk for diabetic retinopathy.
3. Insulin-Resistant Obese Diabetes (IROD)
IROD is a novel cluster seen in India, accounting for 25.9% of cases. Patients in this subgroup display both insulin deficiency and resistance, elevated BMI and waist circumference, and are predisposed to diabetic nephropathy.
4. Combined Insulin Resistant and Deficient Diabetes
Combined Insulin Resistant and Deficient Diabetes is another novel cluster seen in India, comprising 12.1% of cases. These patients manifest early onset of metabolic conditions, with BMI and waist circumference metrics intermediate between SIDD and IROD. They exhibit elevated triglyceride levels and reduced HDL cholesterol and are at an elevated risk for both diabetic nephropathy and retinopathy.
Insulin therapy is commonly prescribed for patients demonstrating an early onset of diabetes mellitus, lower BMI and waist circumference, and higher HbA1C levels despite using multiple OHAs and low C peptide levels.
Secrets to Successful Insulin Therapy
Successful insulin therapy depends on selecting the correct type, technique, titration, timing, testing and tracking of insulin. Let us understand these concepts briefly.
1. Types of Insulin
Insulin can be categorised under two broad subheads: bolus insulin and basal insulin. Bolus insulin (quick-acting insulin) tackles the sudden spike in blood sugar after meals, whereas basal insulin (long-acting insulin) is the residual insulin present in the blood circulation throughout the day.
In an ideal situation, doctors prefer basal-bolus insulin therapy, where they prescribe one shot of basal insulin followed by three shots of bolus insulin.
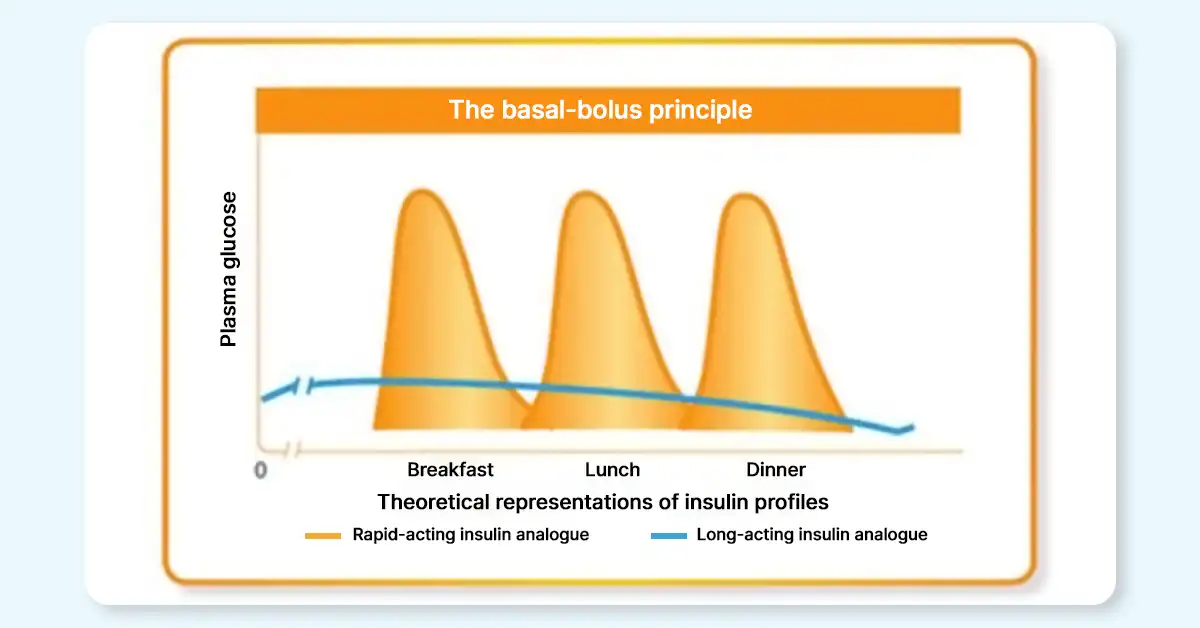
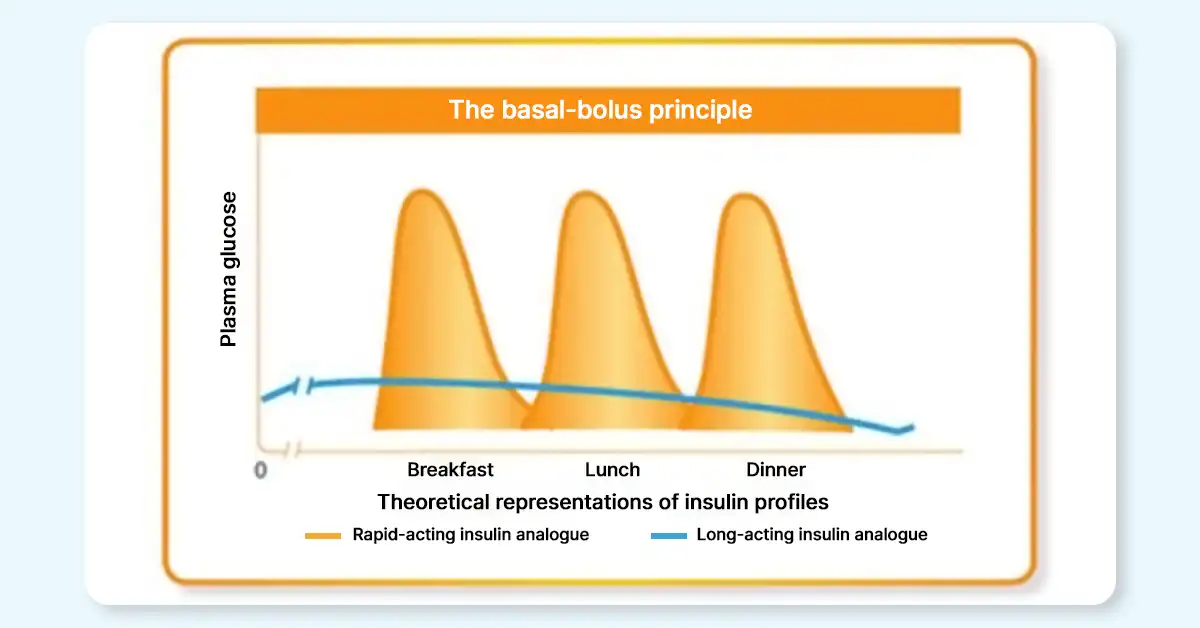
Fig 2: Basal-Bolus Insulin profile
Insulin lispro, aspart, and glulisine are rapid-acting bolus insulins that work quickly to lower blood sugar. They generally reach peak activity within an hour and have a duration of action of approximately 4-5 hours.
Insulin glargine is a basal insulin that has a slow, steady onset and provides coverage for about 24 hours. It’s often administered once daily, although some patients may require twice-daily dosing of this insulin therapy depending on their needs.
Individuals with predominantly high fasting blood sugar require basal insulin therapy, while those with predominantly high post-prandial blood sugar require bolus insulin therapy. For patients experiencing both high fasting and post-prandial blood sugar levels, a basal-bolus regimen or premixed insulin is often prescribed.
Standard premixed formulations usually contain a 30% short-acting and 70% long-acting insulin ratio. In unique cases where post-prandial blood sugar levels are disproportionately elevated compared to already high fasting levels, a 50:50 ratio of short-acting to long-acting insulin may be recommended.
2. Techniques of Delivering Insulin Injections
The technique of administering insulin therapy is as crucial as the selection of the perfect injection for patients. The fastest insulin absorption takes place when injected in the abdominal area, followed by injection in the lateral regions of the thigh.
Also important is to wait for about 5-10 seconds after the injection is complete to ensure that the full dose has been administered before gently removing the pen.
3. Titration of Insulin
Doctors recommend titrating insulin doses via blood sugar monitoring every 2–3 days until glycemic targets are met. For patients on basal insulin, fasting blood sugar (FBS) should be closely monitored. When titrating bolus insulin, post-prandial blood sugar (PPBS) should be the focus of monitoring.
In the case of premixed insulins, it’s important to check FBS, post-breakfast, pre-dinner, and post-dinner blood sugar levels. For younger individuals with diabetes, a target blood sugar range of 90-130 mg/dl is generally effective.
However, older patients with multiple comorbidities may benefit from a more relaxed target. Dose adjustments in insulin therapy, typically in the range of 2-4 units, can help maintain these target levels effectively.
4. Timings of Insulin Injections
Basal insulin is administered at a fixed time every day (usually before bedtime). Rapid-acting bolus insulin should be given 15 minutes before food, while regular bolus insulin should be injected 30 minutes before food. Pre-mixed insulin should also be administered 15-30 minutes before meal.
5. Timely Testing and Tracking of Trends
Diabetologists always advise patients to monitor their blood sugar regularly and track the trend of their glucose levels. For basal insulins, testing the blood sugar pre-meals and for bolus insulin, checking the post-meal sugar is recommended.
For basal-bolus insulin or premixed insulin, both FBS and PPBS should be checked. Tracking the trend of blood sugar levels makes individuals accountable for their health and gain knowledge about preferable and unfavourable foods.
These were some of the important points to keep in mind for gaining expertise in insulin therapy. You can watch the complete discussion in the video below.
About Us
Fitterfly is on a mission to fuel the global metabolic health revolution through the power of Digital Therapeutics (DTx). We partner with physicians to deliver advanced customized digital therapeutics solutions aimed at enhancing the health outcomes of their patients.
By partnering with Fitterfly, you can save time in your clinics, ensure continuity of care for your patients, get research publications and also enhance your revenue. To know more, please fill out the form below or call us at 080-47093933.
This blog provides general information for educational and informational purposes only and shouldn't be seen as professional advice.
Want to know how can Fitterfly enhance your practice and improve patient outcomes?